Managing trauma induced hypothermia within the austere environment
Contents:
Why is hypothermia such a problem in the trauma casualty?
The basics of hypothermia prevention
Challenges within the current systems
Introduction
Hypothermia in the trauma casualty is a common occurrence. It has also been shown that even in high ambient temperatures a significant percentage of trauma casualties become hypothermic during pre-hospital treatment and transport (Bennett BL, 2017). It is well established that hypothermia has a highly detrimental effect on patient outcomes, with mortality in hypothermia combat casualties being double, in comparison to normothermic casualties with similar injuries (Eastridge BJ, 2006 & CPG, 2012). The risk of hypothermia in the trauma casualty is more acute in the austere environment. With exposure to the elements, barriers to prompt treatment, and an increased risk of traumatic injury combining to make hypothermia a major contributor to mortality. Thankfully, innovations in emergency treatment and casualty management technologies are leading to better outcomes for hypothermia casualties, which are explained in this guide. This guide draws upon medical and military research to explain the phenomenon of hypothermia and its specific threats to trauma casualties. It then outlines the current solutions and explains their limitations. An alternative approach, the Xtract™SR Heatsaver from TSG Associates, is explained.
What is hypothermia?
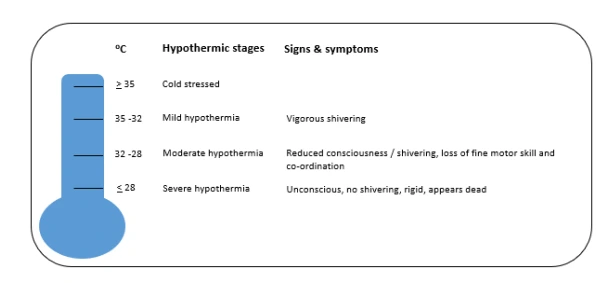
Hypothermia is typically defined when the body’s core temperature drops below 35°C (95℉), and as the temperature continues to fall it can quickly become lifethreatening.
However, in the trauma casualty hypothermic reactions begin once the core temperature is below 36°C (Gentilello L., 1995) making casualties in the austere environment at even greater risk.
The importance of treatment speed
“Due to the physics of heat transfer, hypothermia is far easier to prevent than it is to treat, so prevention of heat loss should begin as soon after wounding as the tactical situation permits” (Defence Health Board, 2010).
Studies show that it is crucial hypothermia is treated immediately. When the body temperature dips to critical levels, receptors that control critical body functions, such as blood pressure quickly start to become dysfunctional, meaning that traditional treatments intended to prevent shock from becoming fatal become less effective. If treatments fail, toxins can build up in the blood. Consequently, when rewarming is subsequently achieved, these toxins are returned to circulation and cause further insult to the casualty.
Why is hypothermia such a problem in the trauma casualty?
Due to the relatively large volume of liquid present in the human body, once a trauma patient is in shock, the ability to reverse hypothermia has been shown to be very difficult (Gentilello L., 1995). Adding to the threat is the loss of platelet clotting capabilities. Hypothermia has a severely detrimental effect on clotting factors, the resulting coagulopathy is a significant contributor in the increased mortality of hypothermic trauma casualties. Along with coagulopathy, acidosis and body temperature forms the so-called ‘triad of death’ (J.Mickhail, 1999). As body temperature falls the mortality rates increase, when core temperature reaches 32°C or below, the mortality rates in trauma casualties is 100%. (J.Jurkovich, 1987 & K.Balvers, 2016).
To ensure the best survival chance for each casualty, normal temperatures must therefore be maintained as a matter of urgency.

The high instances of military Trauma Induced Hypothermia (TIH) have caused alarm. Viewed by the US Department of Defence (DoD) as a trauma system-related problem (Bennett BL, 2017), hypothermia prevention and management is now subject to intervention at a policy level. However, the approach has so far been one that researchers describe as trial and error rather than comprehensive evidence research-based. Currently, the DoD recommends using a combination of Mylar shell systems, heated blankets, vinyl body bags, forced air warming systems, and warmed IV fluids.
The basics of hypothermia prevention
Hypothermia prevention takes many shapes and forms, all of which have the agenda of warming the casualty’s core temperature to within an acceptable range to make him or her receptive to medical intervention and prevent deterioration.
The most commonly used strategies in a remote and austere environment are thin lightweight metalised thermal blankets and shell systems. In this section, we explain why these are so prevalent and their limitations.
1. Mylar blankets & ‘reflective’ shell systems
Developed by NASA in the 1970s, Mylar blankets – also known as ‘space blankets’ – are a familiar component of cold weather kits for the austere environment, in both military and civilian life. The sheets are made of lightweight metalised polyethylene terephthalate (mPET) that claim to reflect around 97% of radiated heat. Cheap to produce, lightweight and easy to carry and deploy in an emergency, these ‘space blankets’ continue to be widely used in situations where hypothermia is a risk and they are frequently carried by people who believe that they could provide protection if trapped outside in conditions that could lead to hypothermia.
Mylar blankets & ‘reflective’ shell systems limitations
Their main limitation is that they require normal body temperatures to be effective. Frequently seen being used by runners after marathons Mylar shells can only reflect the amount of heat that the body gives out, so if an individual is already cold the effectiveness of reflective blankets and shells diminishes. This makes their use limited.
It is often cited that the body loses over 60% of its heat through radiation, however this statistic lacks much credible research to back it up, and is based on healthy, normothermic people.
"Thermal Radiation is the “radiant energy emitted by a medium that is solely due to the temperature of the medium” the temperature of the medium governs the actual emission of thermal radiation" (Gagge, 1966).
A trauma casualty with even moderate hemorrhage undergoes vascular changes (E. Kirkman, 2014) that reduce peripheral blood flow resulting in decreased skin perfusion (M, 2007). This results in cold and damp skin that is much closer to ambient temperature than that of an uninjured normothermic individual. Tipton & Golden in their Essentials of Sea Survival 2013 show that heat loss from radiation when skin is at, or close to, ambient temperature is minimal.
Furthermore, these thin metalised sheets offer almost no insulation with any insulating spaces being easily compressed and they offer a very highly conductive material for heat exchange, allowing any contact with the casualty to lose heat through conduction and convection.
Even the latest iterations of these types of hypothermia mitigation products have the same intrinsic flaws, stemming from the false assertion that heat loss can be reflected back to the casualty (English M, 1990). This demonstrates that heat loss via conduction in supine casualties, was over four times that of heat loss from convection and radiation combined.
“Ensuring that there is insulation between the victim and the ground or the stretcher is a top priority” (Wang H., 2014).
Field-based research shows one major limitation of the currently fielded solution is its lack of insulation. Combat medical personnel have reported that they require supplementary warming systems such as additional insulation and blankets to make the currently fielded hypothermia prevention systems effective. The same researchers noted that the equipment has not been updated since 2006.
2. Forced air warming systems
The forced air warming systems inject warm air through a connecting hose into a quilt-like blanket that has small holes on one surface. Warm air escaping through these holes provides conductive and convective warming to the casualty. The most effective units direct flow toward areas with major blood vessels, like the chest, axilla, abdomen, and groin, where convective heating is most effective.
Forced air warming system limitations
Proven effective, these types of systems are widely used in military and civilian hospitals where they are large requiring a heating unit and pump, large and often impractical storage areas and mains electricity, they lose all efficiency if they become wet, and are therefore designed with clinical settings in mind. The technology is also designed to be operated by specialists, which can be a barrier to field combat use when certain personnel are not present. They are clearly not applicable to the remote austere environment. 3. Additional strategies Comprehensive treatment of hypothermia, especially trauma-induced hypothermia, often includes intensive measures such as heated intravenous (IV) fluids. Although the concept of heating saline, blood, and antibiotic solutions to avoid cooling the body from inside out makes sense on paper, research shows that there is no statistical improvement in core body temperatures compared to the provision of fluids at room temperature. The reasons for this are not clear, and ethical considerations are a significant barrier to comprehensive clinical trials. As such, external warming techniques remain at the forefront of hypothermia prevention. "The rapidity with which rewarming must be accomplished depends on how adversely the hypothermia is affecting the patient. Many techniques serve primarily to maintain endogenously generated heat, and they are ineffective in circumstances during which rapid rewarming is indicated" (Gentilello L., 1995).
3. Additional strategies
Comprehensive treatment of hypothermia, especially trauma-induced hypothermia, often includes intensive measures such as heated intravenous (IV) fluids. Although the concept of heating saline, blood, and antibiotic solutions to avoid cooling the body from inside out makes sense on paper, research shows that there is no statistical improvement in core body temperatures compared to the provision of fluids at room temperature. The reasons for this are not clear, and ethical considerations are a significant barrier to comprehensive clinical trials. As such, external warming techniques remain at the forefront of hypothermia prevention.
"The rapidity with which rewarming must be accomplished depends on how adversely the hypothermia is affecting the patient. Many techniques serve primarily to maintain endogenously generated heat, and they are ineffective in circumstances during which rapid rewarming is indicated" (Gentilello L., 1995).
Tactical Combat Casualty Care (TCCC) and Joint Service Provision (JSP) guidelines for medical personnel
In 2006 the TCCC hypothermia prevention guidelines recommended the use of a commercially available hypothermia prevention and management kit, which was subsequently made readily available to combat personnel. Despite its availability (Lairet JR, 2012) reported that operators frequently selected wool blankets in place of the currently fielded solution to insulate casualties. In June of 2020 TCCC Guidelines changed, recognising the currently fielded systems inability to maintain a thermal balance due primarily to their lack of insulation.
Tactical Combat Casualty Care Guidance
The main focus of the TCCC with regards to hypothermia is hemorrhage management. Due to the lethal triad, blood loss is a primary contributor towards trauma-induced hypothermia. Hypothermia management is listed under Section 7 of the TCCC guidelines. It recommends that casualties are warmed using “readily available insulation,” but gives no specific requirements as to the equipment used to achieve this.
Importantly, TCCC Section 7 states that personnel should “seek to improve upon existing hypothermia enclosure systems when possible,” starkly and formally acknowledging the inherent failures within existing response equipment.
Joint Service Provision (JSP) instructions
Joint Service Provision (JSP) includes hypothermia management as Annex B to JSP 375 Vol 1 C42 (updated 2020). Assessment is required at both group and commander levels, and a primary goal is to prevent additional casualties.
Commanders are instructed to move the casualty indoors, if possible, and to insulate them from the ground. Commanders are also advised to cover the casualty’s head, put the casualty in a sleeping bag, and cover them with blankets. As with JCCC advice, JSP Annex B 375 insists that hypothermic individuals much be “evacuated to medical care as quickly as possible,” revealing the limitations of currently fielded solutions.

Challenges within the current systems
The high incidences of field mortalities resulting from hypothermic trauma illustrate a problem that has yet to be solved. The barriers to success are multiple and challenging.
“Due to the physics of heat transfer, hypothermia is far easier to prevent than it is to treat, so prevention of heat loss should begin as soon after wounding as the tactical situation permits” (DefenseHealthBoard, 2010).
An additional issue is keeping trauma casualties protected from heat loss when medics need access for observations or treatment. The disruption of the equipment used to trap heat can lead to the casualty being exposed to heat loss whilst these interventions are administered.
Efficiency challenges
Practical issues often dictate the efficiency of hypothermic prevention systems in the austere environment as they are required to be compact and lightweight. This has led the drive toward systems that use reflective material as they are relatively compact and lightweight. However, as previously highlighted these ‘reflective shell’ technologies are based on the false premise that lost heat can simply be reflected back to the casualty solving the heat loss problem.
Practical challenges
Under normal circumstances humans lose heat through five mechanisms.
- Convection
- Conduction
- Radiation
- Evaporation
- Respiration
As we have earlier discounted radiation as an insignificant route of heat loss in trauma, let us now look to the remaining four mechanisms to determine how best to improve our care.
Respiration – as cold air is inhaled warmed and exhaled many times a minute this can be a significant source of heat loss and, although methods are available to prewarm the air before it enters the airway, they are typically complicated, bulky and difficult to use when transporting a casualty. However, simple steps such as providing light covering of the nose and mouth may help retain warmth and moisture.
Evaporation – moisture on the skin turned into water vapour is a significant problem for the trauma casualty who is frequently covered in body fluids. The casualty should be dried and placed in a hypothermia mitigation system. Ideally, they should also be placed on a fluid retention pad to try to lock additional fluids away from them to prevent cooling. If using a fluid retaining pad, it must be checked at appropriate intervals to ensure it does not require replacing due to saturation or contamination.
Conduction – likely in many situations to be the most significant route of heat loss is heat loss to the surface when the casualty is resting on the ground.
As recognised in the Casualty Care Guidelines, they should be placed on an insulating surface as quickly as possible to reduce their exposure to direct conductive heat loss. Metalised sheets such as space blankets if allowed to come in direct contact with the casualty may well accelerate heat loss due to the highly conductive nature of the material.
Convection – likely to be the second most significant route to heat loss and often associated with the ‘wind chill factor’. The trauma casualty should be sheltered and protected as much as possible from warm air escaping to whatever insulating system that they are placed in. Opening the system to observe or treat the casualty should be minimised as warm air escaping or cold air entering the system will damage the micro climate that we are trying to establish. Convective heat loss will also be transmitted from the surface of any hypothermia prevention system. A layering insulation system should be used to reduce conduction to the surface of the system where heat can be lost through convection.
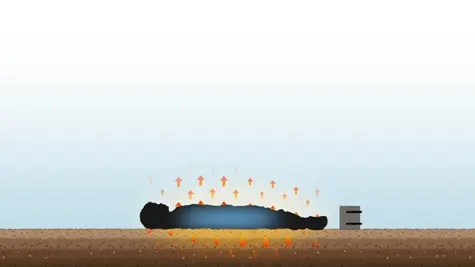
Xtract™SR Heatsaver
A passive insulating system.
This unique product tackles all causes of heat loss within an acceptable size and weight. It is compatible with active heating systems.
- Insulate - Inflatable insulated mattress
- Heatseal - Insulated blanket with fibres concentrated around the body's core
- Element protection sheet - Waterproof top layer

Why it works
The three-stage process of the Xtract™SR Heatsaver works for several reasons:
- The inflatable Insulate mattress provides the insulating layer as recommended by TCCC Guidelines, and removes the casualty from resting directly on the ground, with an uncompressible layer of still air, reducing conductive heat loss to cold surfaces.
- The Heatseal blanket provides an insulating layer on top of the casualty creating tiny pockets of still air that prevent heat loss through both conduction and convection. The majority of the insulation is located around the body’s core and packaged into sculpted thermal insulation panels that hug the body keeping the casualty insulated.
Selective areas can be accessed for treatment, without the need to open and force convention currents through the system.
- The Element Protection Sheet is the waterproof top shell layer which further prevents conduction and convection by providing a windproof and waterproof layer encapsulating the casualty and further reducing heat loss.
Together, the results are comprehensive and offer a dynamic response to casualty insulation.
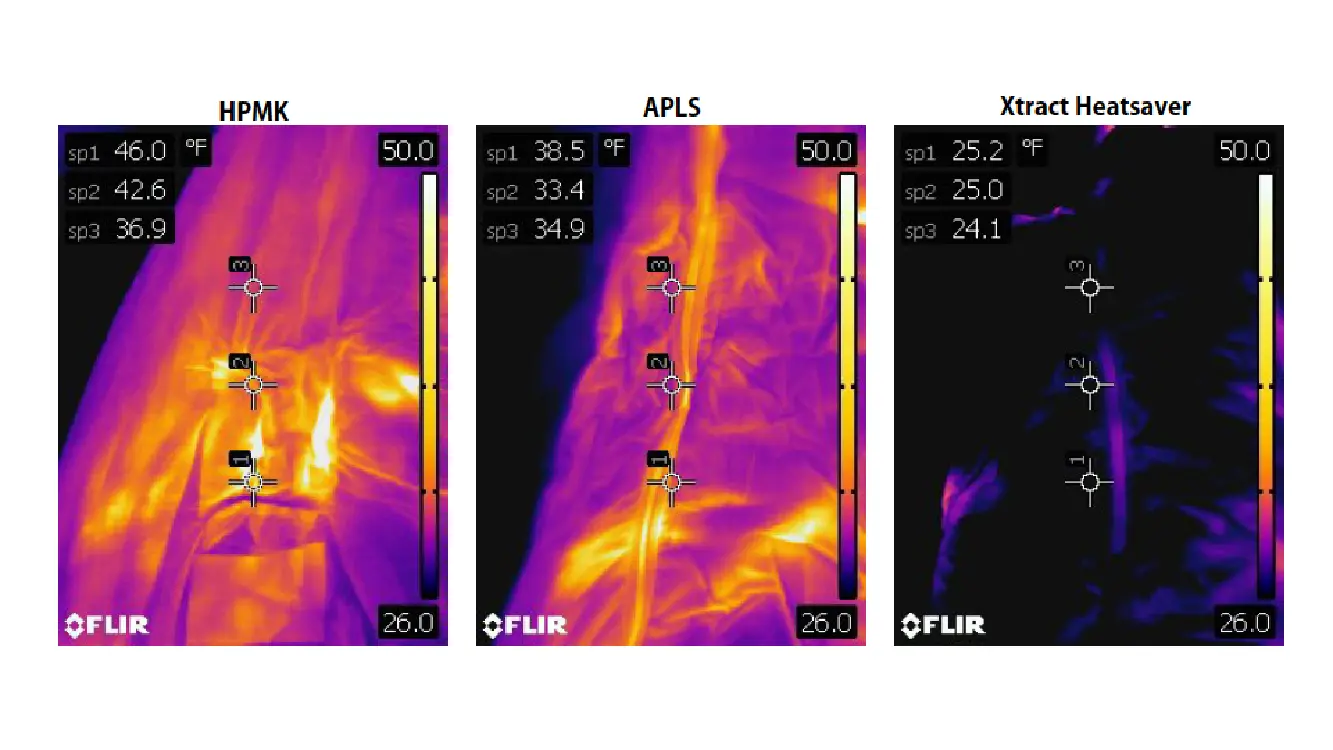
Thermal images of existing hypothermia management solutions and the TSG Associates Xtract™SR Heatsaver
Hypothermia is an enduring threat to the casualty in an austere environment. The Xtract™SR Heatsaver offers many benefits compared to existing solutions and has been designed for its effective, practical, lightweight use in the field.
Contact us for a demonstration
For a demonstration, please call us on 01422 557784 or send us an enquiry via our website.
Get instant access to our guide by confirming your details in the form below:
- Balvers K, Van der Horst M, Graumans M, Boer C, Binnekade JM, Goslings JC, Juffermans NP. Hypothermia as a predictor for mortality in trauma patients at admittance to the Intensive Care Unit. J Emerg Trauma Shock. 2016 JulSep;9(3):97-102. doi: 10.4103/0974-2700.185276. PMID: 27512330; PMCID: PMC4960783.
- Bennett BL, H. J. (2017). Battlefield Trauma-Induced Hypothermia:Transitioning the Preferred Method ofCasualty Rewarming. WILDERNESS & ENVIRONMENTAL MEDICINE, 28, 82-89.
- Committee on Tactical Combat Casualty Care. (2017). TCCC Guidelines for Medical Personnel. Defense Health Board.
- CPG, J. (2012). Hypothermia Prevention, Monitoring, and Management. JFJones. Danks, R. (2002). Triangle of Death. How Hypothermia Acidosis & Coagulopathy Can Adversely Impact Trauma Patients. JEMS, 27(5), 61-70.
- DefenseHealthBoard. (2010). Recommendations Regarding the TCCC Guidelines on the Prevention of Hypothermia. Defense Health Board.
- E. Kirkman, S. W. (2014). Haemodynamic changes in trauma. British Journal of Anaesthesia, 226-275.
- Eastridge BJ, J. D. (2006). Trauma system development in a theater of war: experiences from Operation Iraqi Freedom and Operation Enduring Freedom. Journal of Trauma, 61, 1366-1372.
- English MJ, Farmer C, Scott WA. Heat loss in exposed volunteers. J Trauma. 1990 Apr;30(4):422-5. PMID: 2325172.
- Gagge. (1966). Mechanisms of heat exchange, Radiation Heat Transfer. Belmont CA: Wadsworth.
- Gentilello L., M. S. (1995). Treatment of Hypothermia in Trauma Victims: Thermodynamic Considerations. J Intensive Care Med, 5-14.
- Golden FS, Tipton M (2002), “Essentials of Sea Survival” Human Kinetics ISBN:0- 7360-0215-4 https://www.researchgate.net/publication/270283180_Essentials_of_Sea_Survival Golden FS, Francis TJ, Gallimore D, Pethybridge R. Lessons from history: morbidity of cold injury in the Royal Marines during the Falklands Conflict of 1982. Extrem Physiol Med. 2013 Aug 8;2(1):23. doi: 10.1186/2046-7648-2-23. PMID: 24070118; PMCID: PMC3750324.
- JM Johnson (2007). Mechanisms of vasoconstriction with direct skin cooling in humans. Am J Physiol Heart Circ Physiol. 2007 Apr;292(4):H1690-1. doi: 10.1152/ajpheart.00048.2007. Epub 2007 Jan 19. PMID: 17237255.
- Jurkovich GJ, Greiser WB, Luterman A, Curreri PW. Hypothermia in trauma victims: an ominous predictor of survival. J Trauma. 1987 Sep;27(9):1019-24. PMID: 3656464.
- Lairet JR, B. V. (2012). Prehospital interventions performed in combat zone: a prospective multicenter study of 1003 combat wounded. J Trauma Acute Care Surg., s38-s42.
- Mikhail, J. (Feb 1999), "The trauma triad of death: hypothermia, acidosis, and coagulopathy", AACN Clin Issues, 10 (1): 85–94, doi:10.1097/00044067- 199902000-00008, PMID 10347389, S2CID 28587725
- Wang H., H. J. (2014). Research progress on combat trauma treatment in cold regions. Military Med Res, 8.